Working Papers and Selected Works in Progress
Competition in Employer Sponsored Health Insurance: Implications for a Public Option
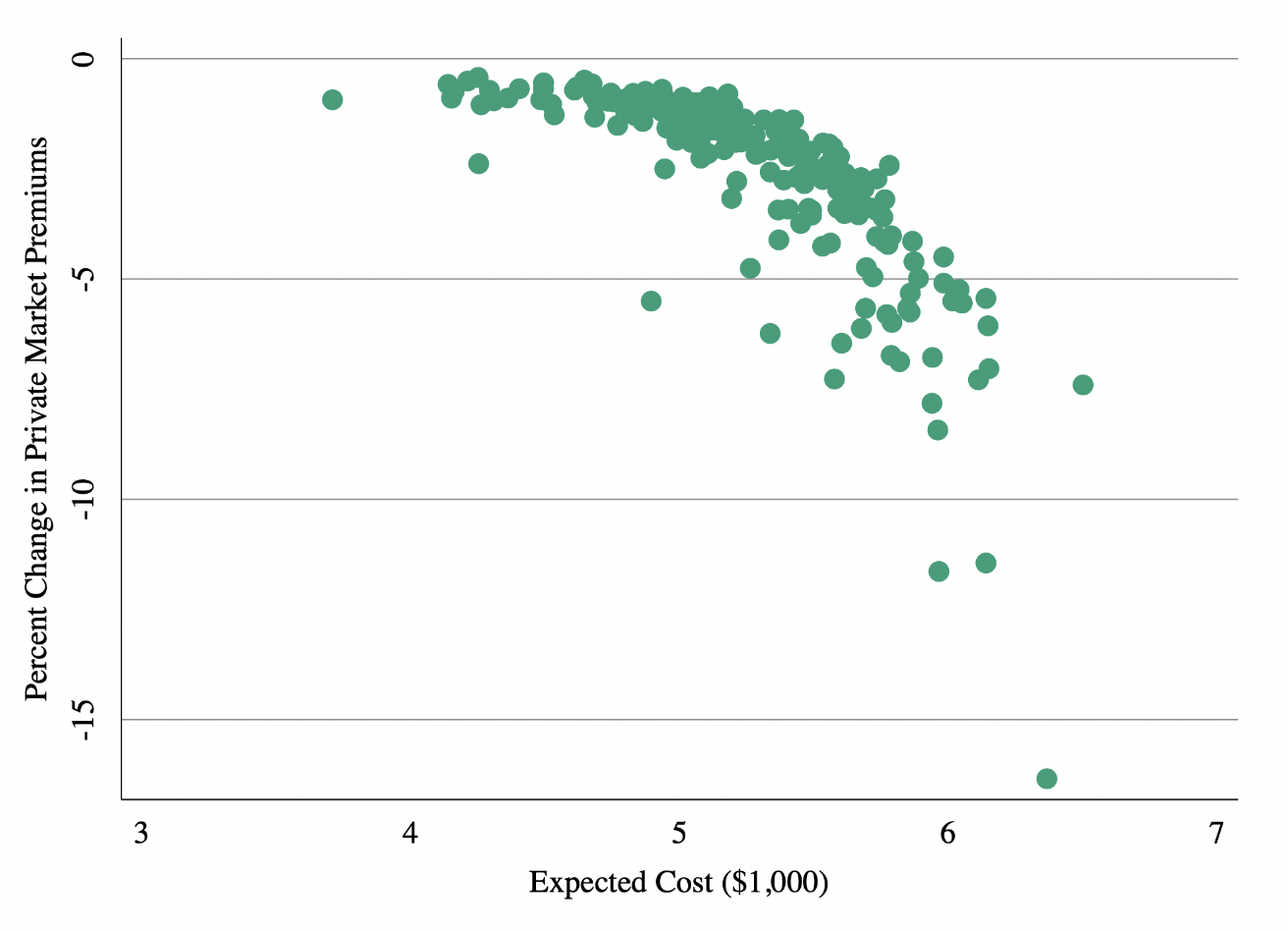
I explore the conditions under which a government insurance plan, or “public option,” generates additional premium competition in the insurance market. Using unique data on employer-insurer contracting and a model of supply and demand, I document evidence of large switching costs and variation in expected costs across employers. Insurers respond to switching costs by setting low premiums for new employers and raising them for those who are locked-in. I use the model to test the impact of a public option and show show that uniform premium setting (i.e. community rating) substantially limits the public option’s ability to compete with private insurers who set employer-specific premiums. A public option that offers experience rated premiums and discounts to new employers is substantially more attractive and therefore has a larger impact on premium competition. A community rated public option that aggressively regulates prices for health care services obtains substantial market share, but is less effective at generating competition among existing insurers.
Who Pays for Rising Health Care Prices? Evidence from Hospital Mergers, with Zarek Brot-Goldberg, Zack Cooper, Lev Klarnet, Ithai Lurie, and Corbin Miller. NBER Working Paper 32613. Revisions Requested at AER
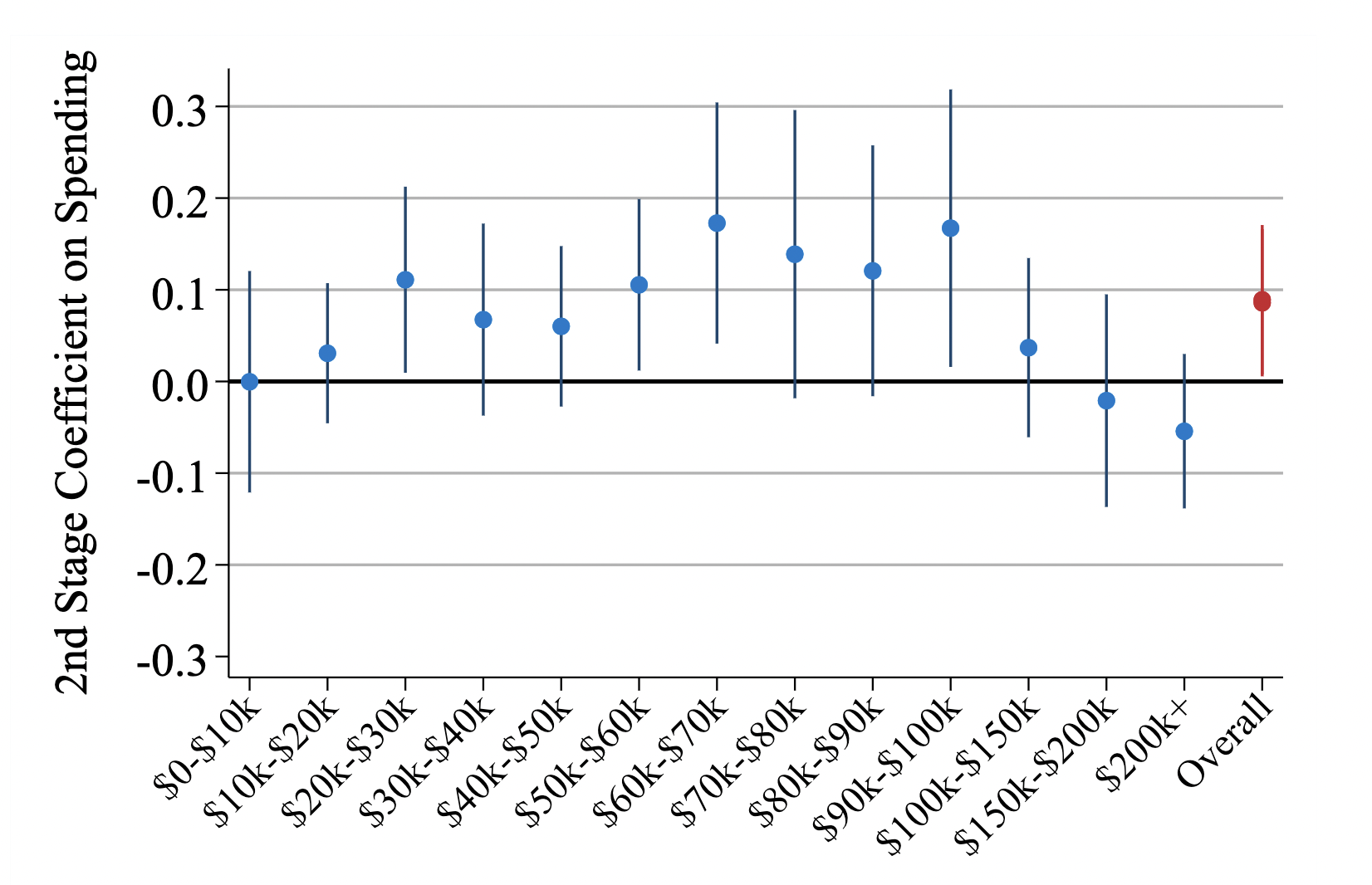
We analyze the economic consequences of rising health care prices in the US. Using exposure to price increases caused by horizontal hospital mergers as an instrument, we show that rising prices raise the cost of labor by increasing employer-sponsored health insurance premiums. A 1% increase in health care prices lowers both payroll and employment at firms outside the health sector by approximately 0.4%. At the county level, a 1% increase in health care prices reduces per capita labor income by 0.27%, increases flows into unemployment by approximately 0.1 percentage points (1%), lowers federal income tax receipts by 0.4%, and increases unemployment insurance payments by 2.5%. The increases in unemployment we observe are concentrated among workers earning between $20,000 and $100,000 annually. Finally, we estimate that a 1% increase in health care prices leads to a 1 per 100,000 population (2.7%) increase in deaths from suicides and overdoses. This implies that approximately 1 in 140 of the individuals who become fully separated from the labor market after health care prices increase die from a suicide or drug overdose.
Are Hospital Acquisitions of Physician Practices Anticompetitive?, with Zack Cooper, Matthew Grennan, Joseph Martinez, Fiona Scott Morton, and Ashley Swanson
Health Care Spending Effects of Patients, Providers, and Places: Evidence from the Military Health System, with Amy Bond and Steve Schwab
Published Papers
Economics
Is There Too Little Antitrust Enforcement in the U.S. Hospital Sector? American Economic Review: Insights, 2024, with Zarek Brot-Goldberg, Zack Cooper, and Lev Klarnet
Final pre-print: April, 2024
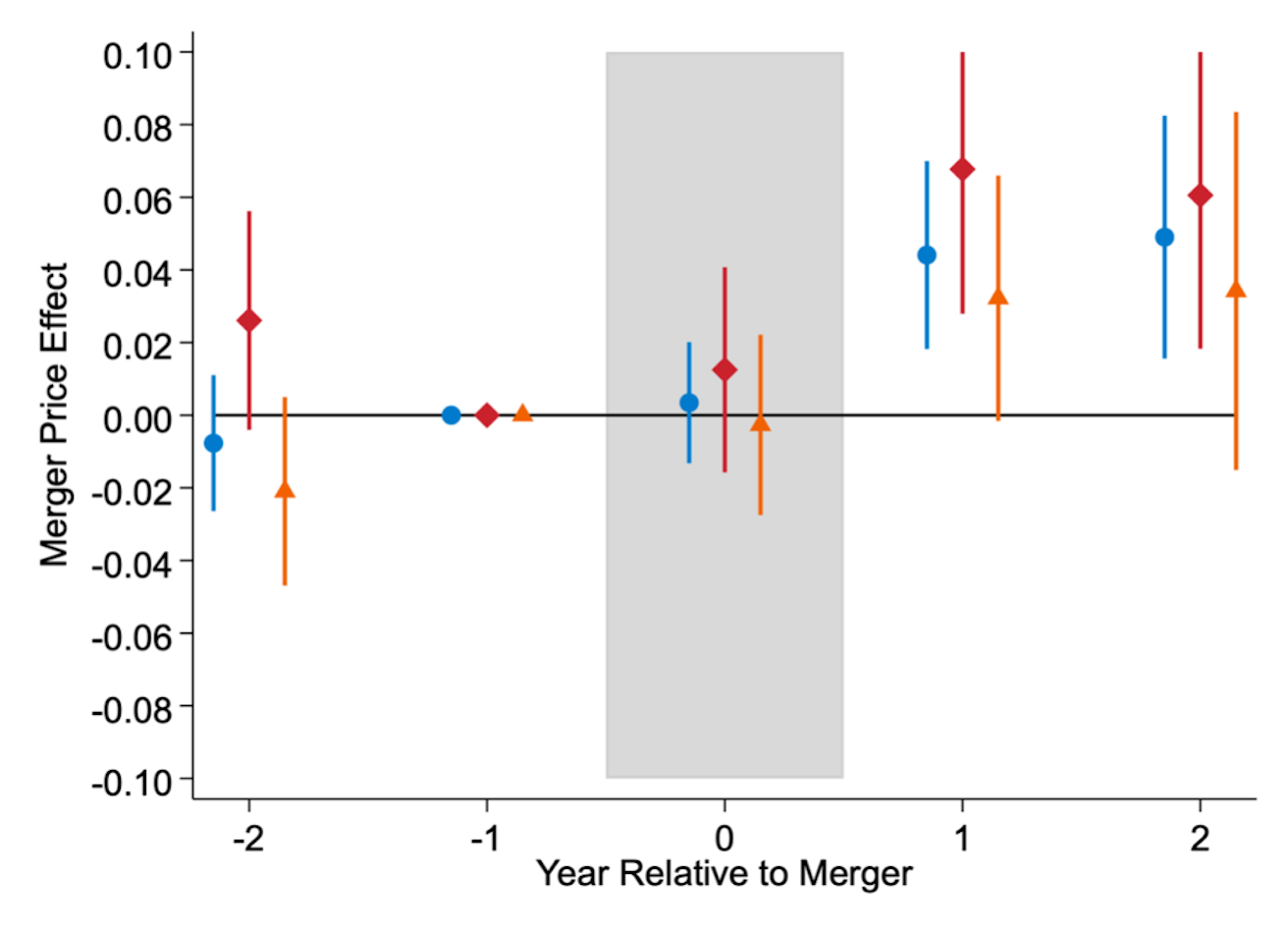
From 2002 to 2020, there were over 1,000 mergers of US hospitals. During this period, the Federal Trade Commission (FTC) took enforcement actions against 13 transactions. However, using the FTC’s standard screening tools, we find that 20% of these mergers could have been predicted to meaningfully lessen competition. We then show that, from 2010 to 2015, predictably anticompetitive mergers resulted in price increases over 5%. We estimate that approximately half of predictably anticompetitive mergers had to be reported to the FTC per the Hart-Scott-Rodino Act. We conclude that there appears to be underenforcement of antitrust laws in the hospital sector.
Press: WSJ, Axios, Stat, Modern Healthcare
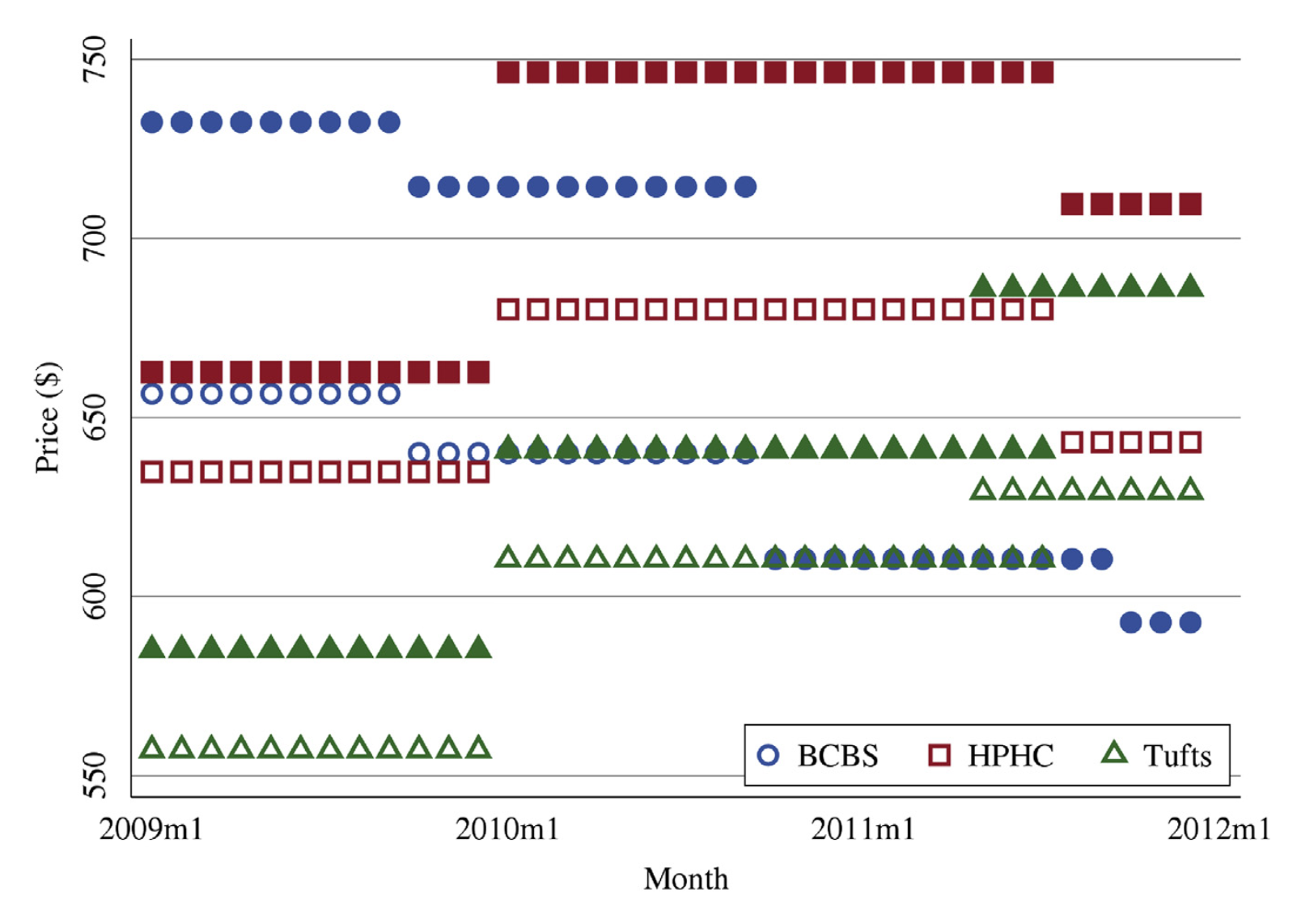
How Important Is Price variation Between Health Insurers? Journal of Health Economics, 2021, with Keith Ericson and Amanda Starc
Prices negotiated between payers and providers affect a health insurance contract’s value via enrollees’ cost-sharing and self-insured employers’ costs. However, price variation across payers is difficult to observe. We measure negotiated prices for hospital-payer pairs in Massachusetts and characterize price variation. Between-payer price variation is similar in magnitude to between-hospital price variation. Administrative-services-only contracts, in which insurers do not bear risk, have higher prices. We model negotiation incentives and show that contractual form and demand responsiveness to negotiated prices are important determinants of negotiated prices.
Press: WSJ
Mergers and Marginal Costs: New Evidence from Hospital Input Markets, RAND Journal of Economics, 2021, with Matthew Grennan and Ashley Swanson
We estimate the effects of hospital mergers, using detailed data containing medical supply transactions (representing 23 percent of operating costs) from a sample of US hospitals 2009-2015. Pre-merger price variation across hospitals (Gini coefficient 7 percent) suggests significant opportunities for cost decreases. However, we observe limited evidence of actual savings. In this retrospective sample, targets realized 1.9 percent savings; acquirers realize no significant savings. Examining treatment effect heterogeneity to shed light on theories of "buyer power," we find that savings, when they occur, tend to be local, and potential benefits of savings may be offset by managerial costs of merging.
The Price Ain’t Right? Hospital Prices and Health Spending on the Privately Insured, Quarterly Journal of Economics, 2019, with Zack Cooper, Martin Gaynor, and John Van Reenen
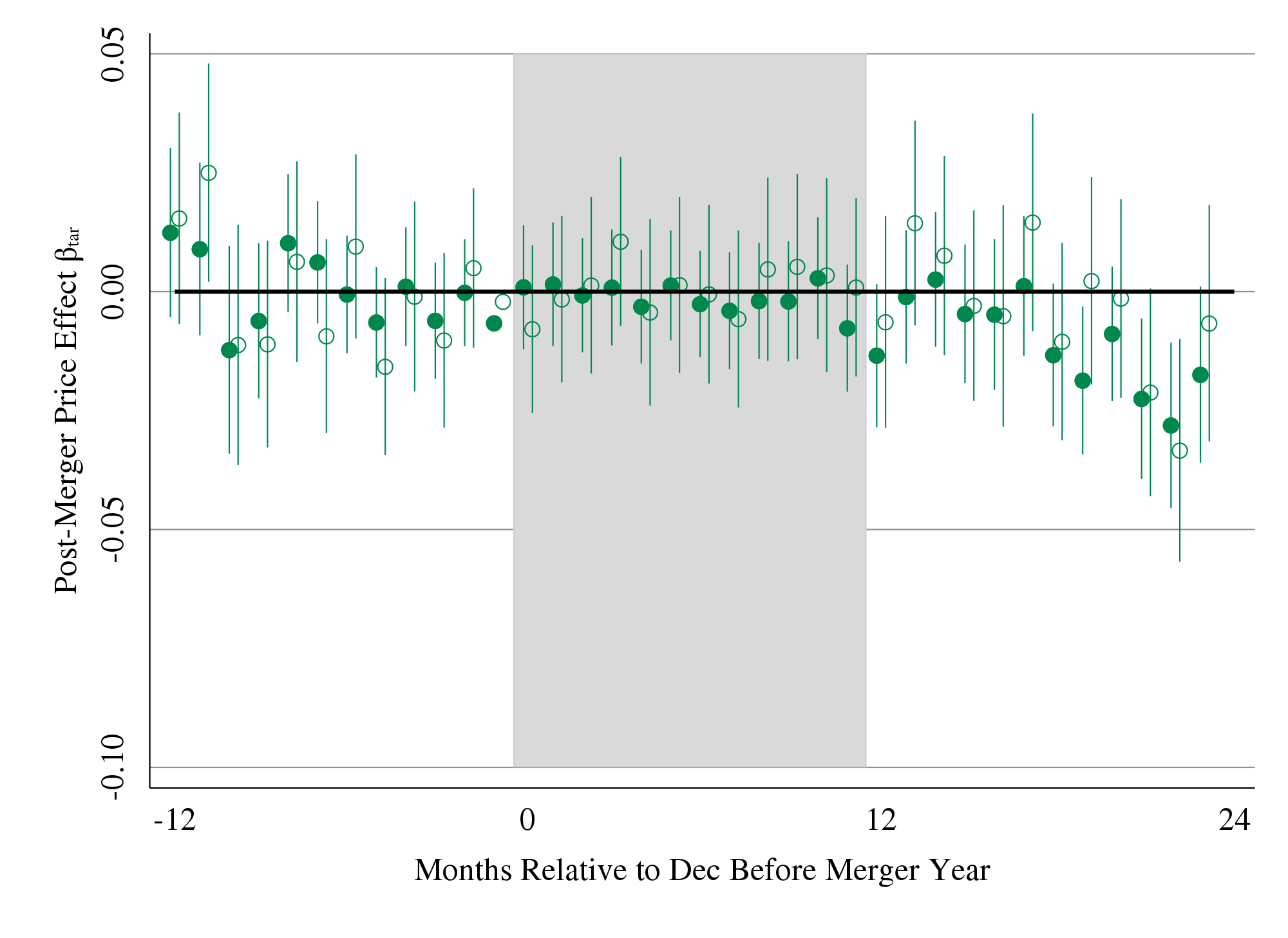
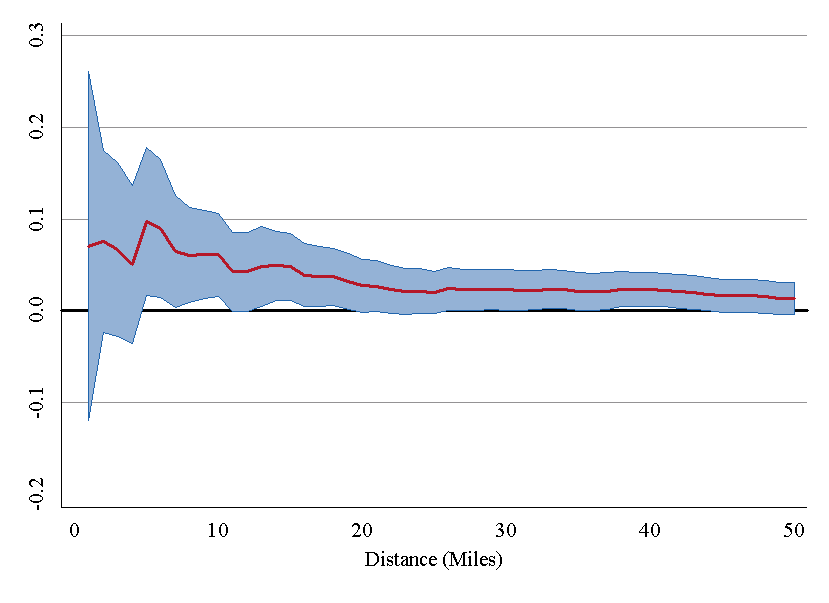
We use insurance claims data to study the variation in health spending on the privately insured, examine the structure of insurer-hospital contracts, and analyze the variation in hospital prices across the nation. Prices vary substantially across regions, across hospitals within regions, and even within hospitals. Hospital market structure is strongly associated with price levels and contract structure. Prices at monopoly hospitals are 12% higher than those in markets with four or more rivals. Monopoly hospitals also have contracts that load more risk on insurers. In concentrated insurer markets the opposite occurs—hospitals have lower prices and bear more financial risk. Examining the 366 mergers and acquisitions that occurred between 2007 and 2011, we find that prices increased by over 6% when the merging hospitals were geographically close (e.g., 5 miles or less apart), but not when the hospitals were geographically distant (e.g., over 25 miles apart).
Press: NYT, WSJ, New Yorker, NPR Marketplace, Vox, More links here
Health, Policy, Measurement
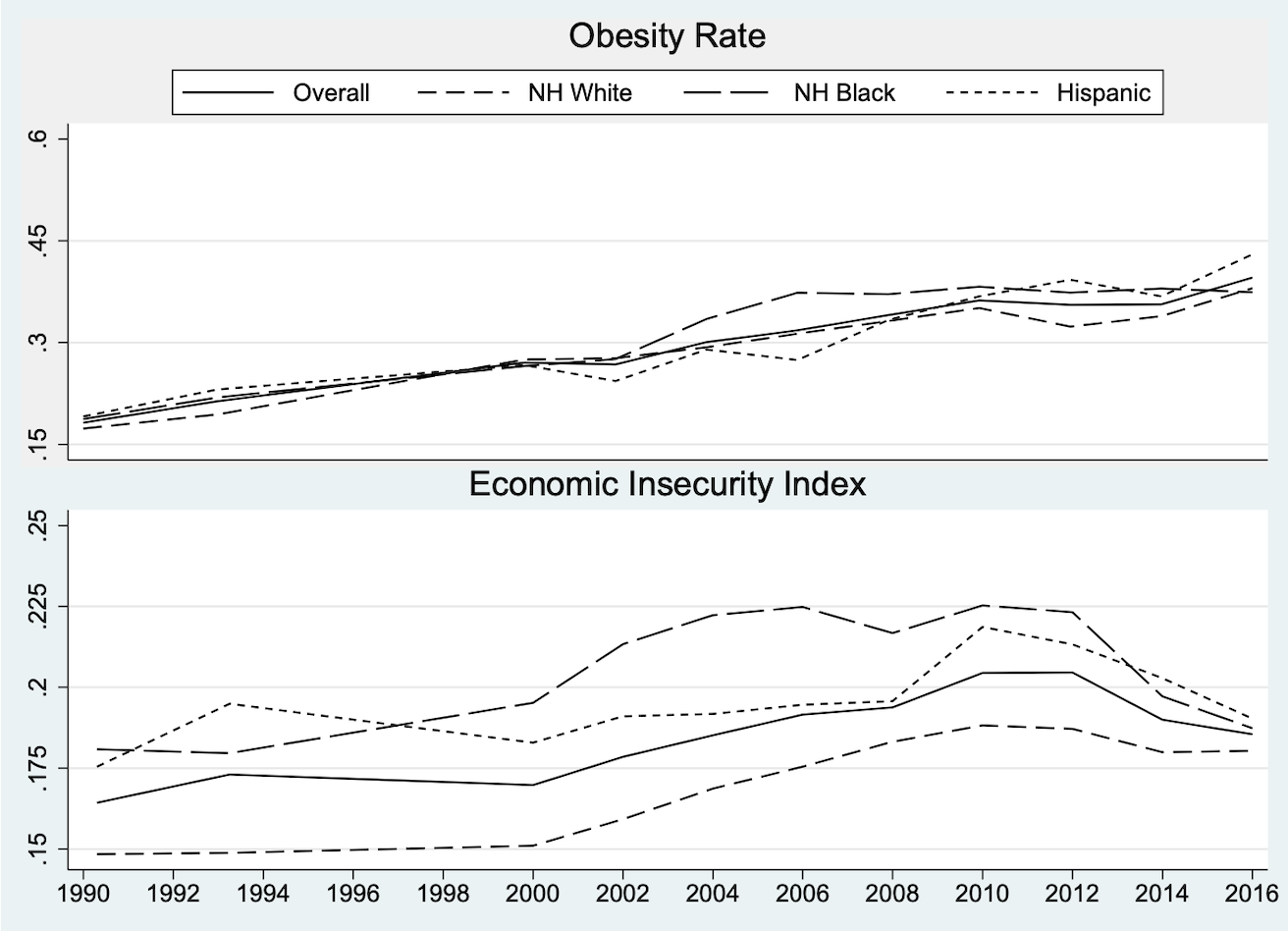
'Rational Overeating' in a Feast-or-Famine World: Economic Security and the Obesity Epidemic, Southern Economic Journal, 2023, with Trenton G. Smith and Steven Stillman
We investigate the potential role of economic insecurity - the extent to which a household faces the threat of catastrophic income loss — in explaining these changes. We construct a synthetic panel of demographic groups for 1988–2016 by combining the Economic Security Index (which measures the probability of a year-on-year drop in adjusted household income of 25% or more) with data from the NHANES surveys. We find robust evidence of a link between economic insecurity and obesity, suggesting a nearly one-to-one correspondence in percentage point changes in ESI and obesity, for both men and women.
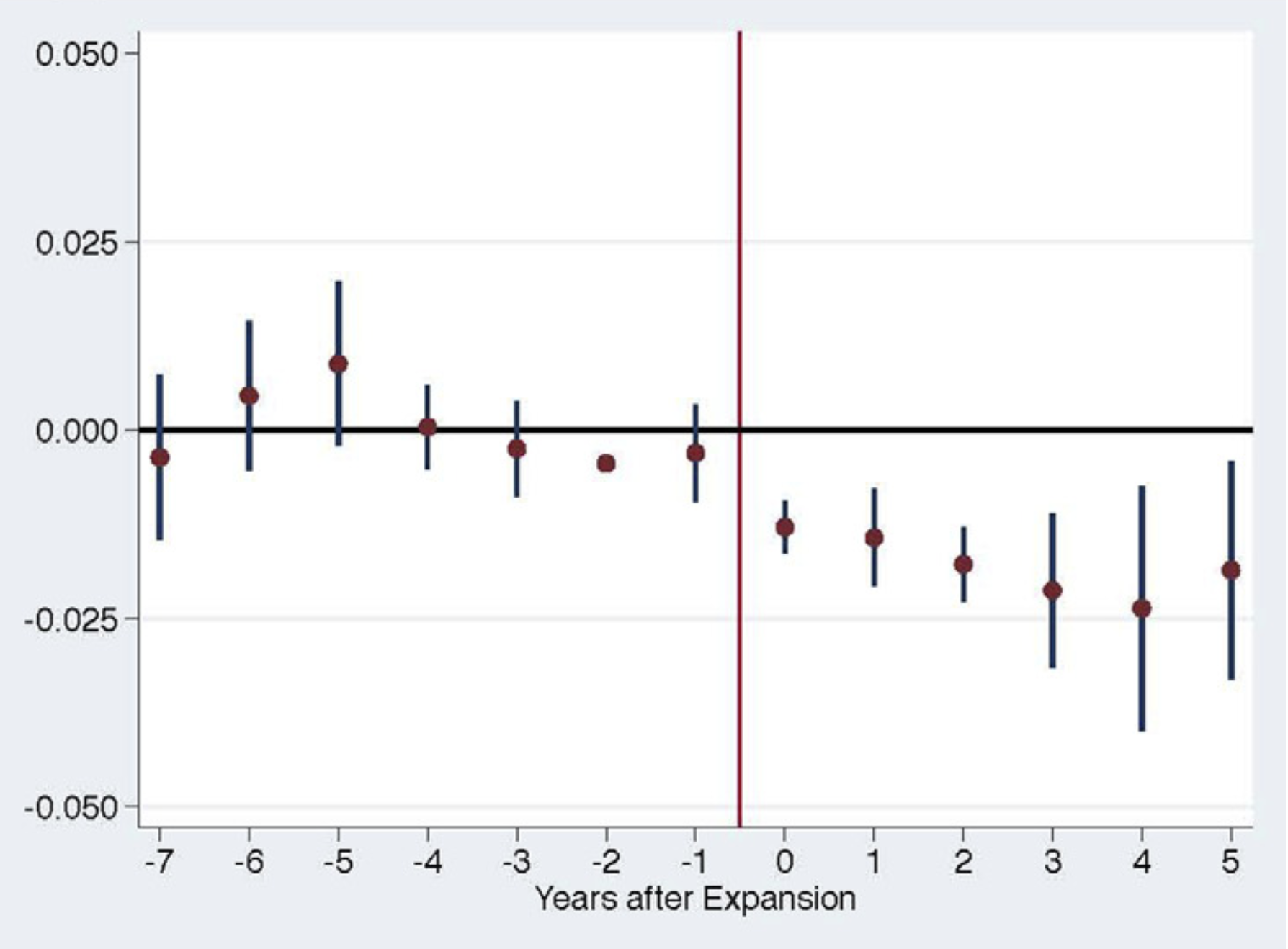
Impact of Medicaid Expansion on Women with Gynecologic Cancer: a Difference-in-Difference Analysis, American Journal of Obstetrics and Gynecology, 2020, with Benjamin B. Albright, Dimitrios Nasioudis, Haley A. Moss, Nawar A. Latif, Emily M. Ko, and Ashley F. Haggerty
Using data from the National Cancer Database, we study the impact of state-level policy to expand Medicaid on access to care for women with gynecologic cancer. Using a difference-in-difference approach, we find that states that expanded Medicaid reduced the rate of uninsurance at diagnosis by 2pp. Medicaid expansion also generated a 0.8pp increase in early stage diagnosis, a 1.62 pp increase in treatment within 30 days of diagnosis, and 1.54pp incrase in surgery within 30 days of diagnosis. We estimate particularly large gains for women living in low-income zip codes, Hispanic women, and women with cervical cancer.
Variation In Health Spending Growth For the Privately Insured From 2007 to 2014, Health Affairs, 2019, with Zack Cooper, Charles Gray, Martin Gaynor, and John Van Reenen
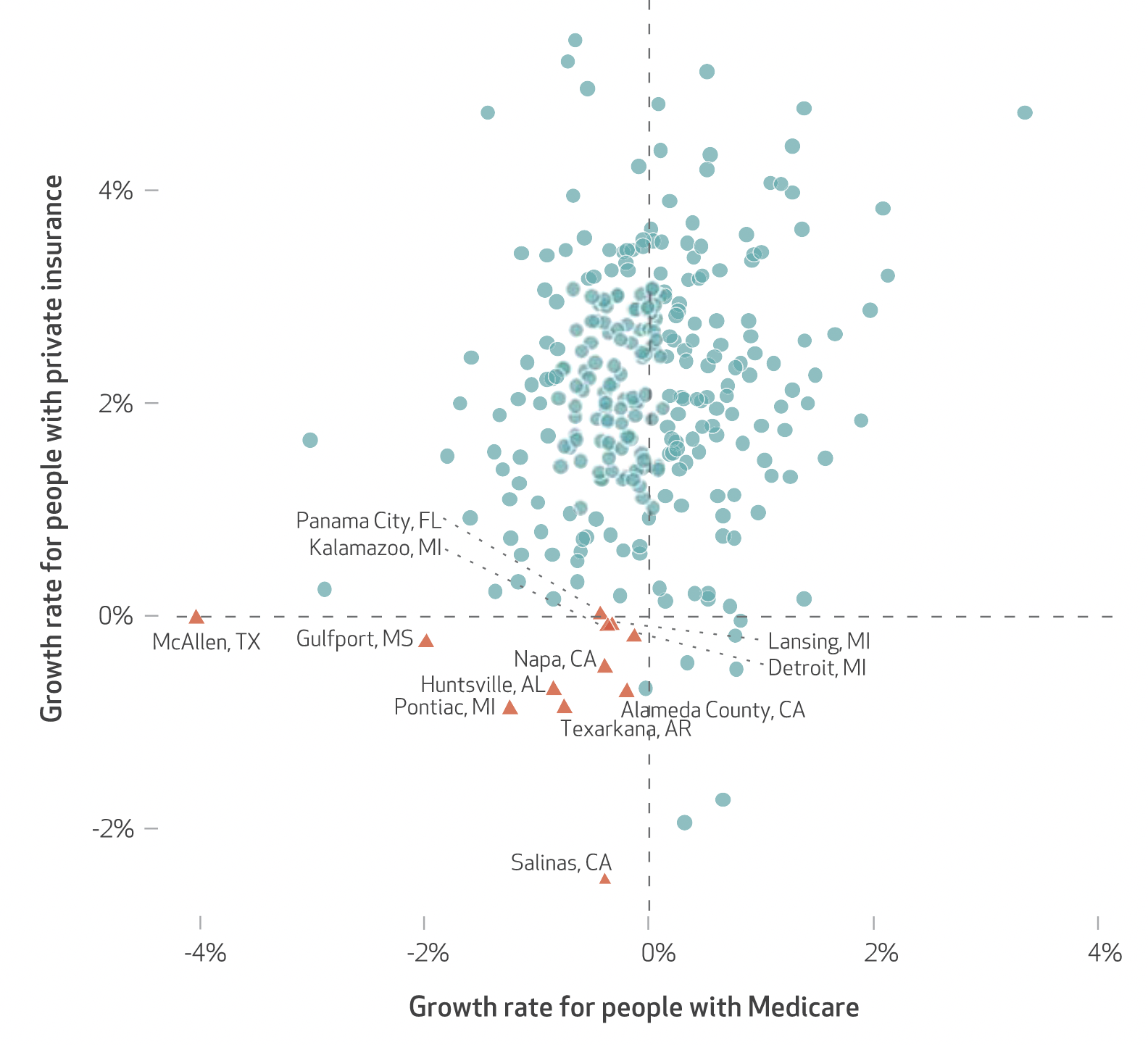
We examined the growth in health spending on people with employer-sponsored private insurance in the period 2007–14. In the study period private health spending per enrollee grew 16.9 percent, while growth in Medicare spending per fee-for-service beneficiary decreased 1.2 percent. There was substantial variation in private spending growth rates across hospital referral regions (HRRs): Spending in HRRs in the tenth percentile of private spending growth grew at 0.22 percent per year, while HRRs in the ninetieth percentile experienced 3.45 percent growth per year. The correlation between the growth in HRR-level private health spending and growth in fee-for-service Medicare spending in the study period was only 0.211, suggesting that different factors may be driving the growth in spending on the two populations.
Press: Modern Healthcare
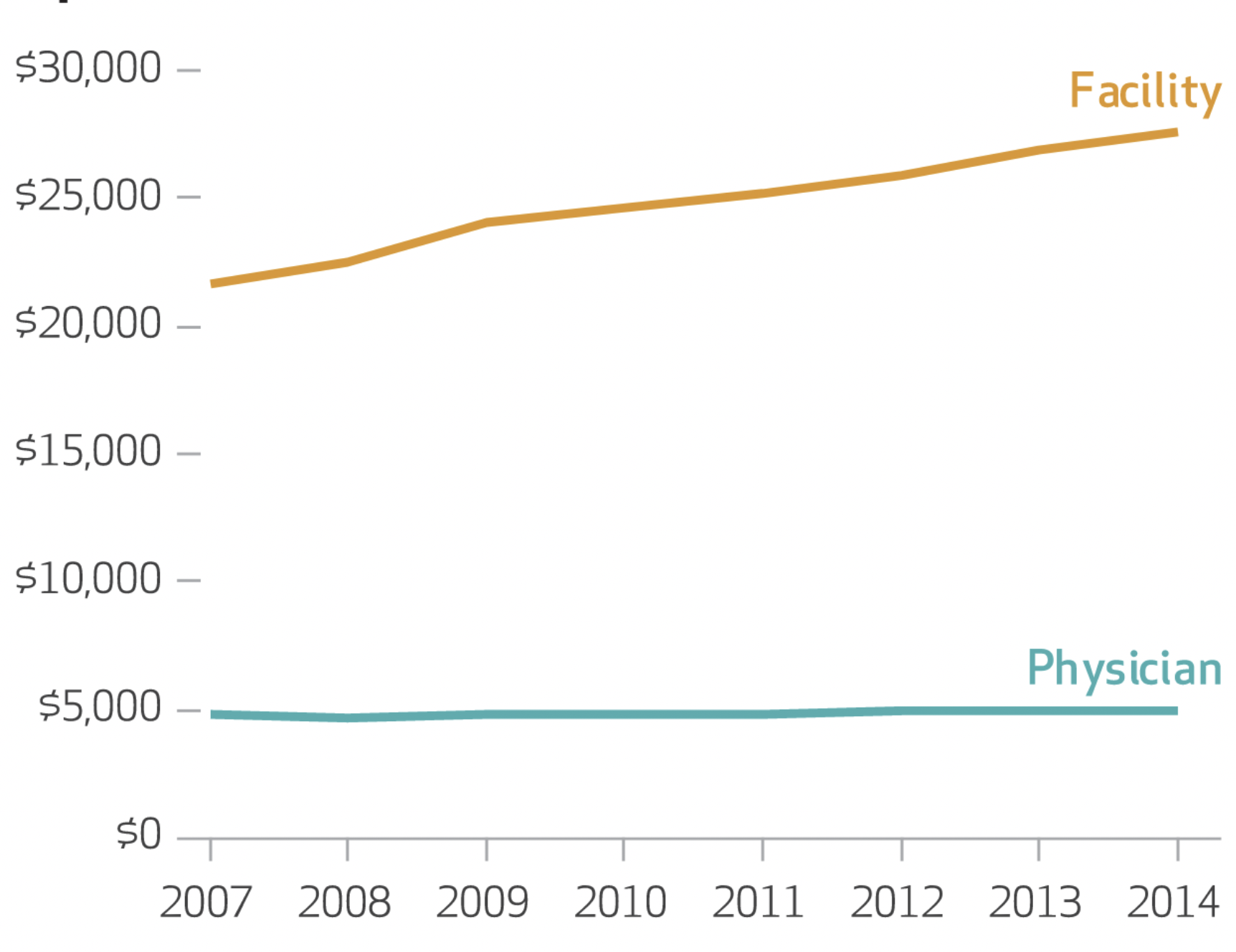
Hospital Prices Grew Substantially Faster Than Physician Prices For Hospital-Based Care In 2007-2014, Health Affairs, 2019, with Zack Cooper, Martin Gaynor, Nir J. Harish, Harlan M. Krumholz, and John Van Reenen
We analyzed growth in both types of prices for inpatient and hospital-based outpatient services using actual negotiated prices paid by insurers. We found that in the period 2007–14 hospital prices grew substantially faster than physician prices. For inpatient care, hospital prices grew 42 percent, while physician prices grew 18 percent. Similarly, for hospital-based outpatient care, hospital prices grew 25 percent, while physician prices grew 6 percent. Policy makers should consider a range of options to address hospital price growth, including antitrust enforcement, administered pricing, the use of reference pricing, and incentivizing referring physicians to make more cost-efficient referrals.
Press: Modern Healthcare
The Economic Security Index: A New Measure for Research and Policy Analysis The Review of Income and Wealth, 2014, with Jacob S. Hacker, Gregory A. Huber, Austin Nichols, Philipp Rehm, Mark Schlesinger, and Robert G. Valletta
The ESI assesses the individual-level occurrence of substantial year-to-year declines in available household resources, accounting for fluctuations not only in income but also in out-of-pocket medical expenses. It also assesses whether those experiencing such declines have sufficient liquid financial wealth to buffer against these shocks. We find that economic insecurity has risen steadily since the mid-1980s for virtually all sub-groups of Americans, though there is substantial disparity in the degree to which different subgroups are exposed to economic risk. We find that the degree and disparity by which insecurity has risen is robust across the best available data sources.

Press: Lots of links here
